‘I Was the First To Get the COVID-19 Vaccine, But So Many Other Black People Distrust It’—Here’s Why
For many Black people, distrust of the COVID-19 vaccine, and the medical system as a whole, is a product of lived experience.
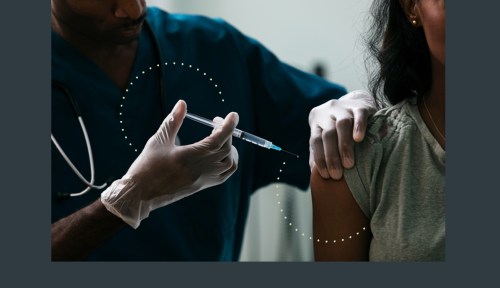
Black Americans are disproportionately hospitalized for and dying from COVID-19, but the community has shown less inclination to be vaccinated than other racial and ethnic groups, according to a report from the Pew Research Center. So, when nurse Sandra Lindsay, MS, RN, who is Black, became the first person in the United States to receive the COVID-19 vaccine outside of a clinical trial, she knew that sharing her positive experience might make others more willing to get vaccinated. That’s because she understands the hesitancy, which stems from centuries of trauma and abuse at the hands of medical professionals who have shown they can not be trusted.
Experts in This Article
biochemist, neurobiologist, antibody engineer, and senior scientist at GlaxoSmithKline.
Harriet A. Washington is a science writer, ethicist, and researcher. She is the author of Infectious Madness, Deadly Monopolies, and Medical Apartheid .
James Hildreth, PhD, MD, is an immunologist and the president and CEO of Meharry Medical College.
Michelle Chester, DNP, is the corporate director of employee health services at Northwell Health.
Sandra Lindsay, MS, RN, is the director of nursing for critical care at Long Island Jewish Medical Center. She is the first person in the U.S to receive the COVID-19 vaccine outside of a clinical trial.
“We’ve never really completely reconciled that distrust. What we need to do moving forward is to not dismiss that this distrust is valid and real, because it’s based on evidence,” says Lindsay, who is the director of nursing for critical care at Long Island Jewish Medical Center. Overcoming the issue will take time. “Our leaders need to prioritize it, acknowledge it, and just keep working at it. It’s not going to happen overnight.”
The evidence
In discussions of the Black community’s mistrust of medicine, experts often bring up the example of the Tuskegee Syphilis Experiment, a 40-year study that allowed hundreds of Black men to go untreated for syphilis despite treatment for the disease becoming available some 15 years into the study. But science writer, ethicist, and researcher Harriet A. Washington says that for most people, the Tuskegee experiment has nothing to do with it. “I can’t stress that enough,” she says. In fact, a 2005 study by Thomas LaVeist, PhD, found that most Black people interviewed did not know about the experiment and that knowledge of it did not directly link to distrust of the medical system. Their mistrust isn’t a product of one study—but of lived experience.
“If you can claim that people are reacting to a single study, the implication is that African Americans are overreacting to one study rather than African Americans are logically reacting to four centuries of abuse,” says Washington. “Those are two very different things.”
Washington’s book Medical Apartheid delves deeper into the history, unpacking 400 years of abuse that Black Americans have faced at the hands of physicians. It shares how the practice of gynecology came out of anesthesia-free experiments on enslaved women. Radiation experimentation was involuntarily performed on many American civilians, most of whom were Black, during World War II through the Manhattan Project. And Black children weren’t spared: In the 1990s, they were test subjects in a New York Psychiatric Institute study of the now-banned diet drug fenfluramine.
“It was not just a matter of a hoary history. It’s a matter of things that just happened a few months ago.”
In fact, just last year, two French doctors came under fire for suggesting COVID-19 vaccine trials could be run on prostitutes in Africa. “In April, you had researchers saying, ‘Let’s do this COVID research in Africa with Black people,'” says Washington. “Now it’s a few months later, and you wonder [why] they’re not flocking to line up for vaccines? It was not just a matter of a hoary history. It’s a matter of things that just happened a few months ago.”
In addition to their mistreatment in medical studies, Black people continue to face systemic racism in their day-to-day interactions with physicians. For example, a 2016 study conducted by researchers at the University of Virginia found that some white doctors still believed there were biological differences between Black and white people, and that these racial biases informed their medical judgments and could influence the way they assessed their patients’ pain and treated them. And the number of pregnancy-related deaths per 100,000 people is 3.2 times higher for those who are non-Hispanic Black than for those who are white.
“It’s frankly illogical to ask people who’ve been repeatedly abused in the health-care system to then blindly trust it,” says Washington. But, with the COVID-19 pandemic continuing to ravage the nation, Washington says she understands the sense of urgency behind garnering this trust. A report from Pew Research Center that was released in December 2020 showed that only 42 percent of Black people surveyed intended to get vaccinated, compared to 83 percent of English-speaking Asian Americans, the group most willing to take the vaccine.
Gaining trust
Immunologist and president and CEO of Meharry Medical College James Hildreth, PhD, MD, who is Black, says he hopes to see his community, which is dying from COVID-19 at a rate 2.8 times higher than that of white people, come around to the vaccine.
“There’s ample reason for people in our communities to have some mistrust of the medical research apparatus,” says Dr. Hildreth. “And if we’re going to be successful in fighting COVID-19 in our communities we have to get past that somehow. Being able to explain the science behind vaccines, why they work, how they work, and why it’s so important that we be a part of the studies is the approach that I’m trying to take as someone who’s been studying viruses and vaccines for decades.”
By sharing his knowledge and experience, Dr. Hildreth hopes he can persuade more people to trust that the vaccine is safe and effective. For example, he wants people to know that even though the vaccine trial happened faster than they usually do, that doesn’t mean they were rushed. “Whoever it was who decided to call the vaccine Operation Warp Speed kind of did us a disservice, because it implies that perhaps in the rush to develop a vaccine some important steps in evaluating them would be omitted,” says Dr. Hildreth. “As far as I know, and I’m not privy to all of it, none of the steps required to safely evaluate a vaccine are being omitted. It’s just that some of the steps are being run in parallel, so you can get there faster.” This, he adds, is a more costly process but not necessarily a less effective one.
“Instead of talking about African American behavior, we need to talk about the health-care system.”
Other Black doctors are hoping their personal involvement will help to persuade patients to get vaccinated. Michelle Chester, DNP, the doctor who administered the vaccine to Lindsay, says she has been working with her church to get the word out. “I’m a big advocate at my church and the chairperson for the health ministry,” says Dr. Chester, who is the corporate director of employee health services at Northwell Health. “And because I’ve done that, there’s so much trust now with the education that I’ve done. So I think that’s somewhere where we can start.”
Representation also helps. The fact that the first doctor to administer the COVID-19 vaccine in the U.S. was black—as were the first and second people to receive it—could have been beneficial: Research has shown that Black people are more inclined to trust their doctors and more likely to have better health outcomes when their doctors are also Black.
But what if a Black patient can’t find a doctor who shares their racial heritage—someone they feel they can trust? As beneficial as the vaccination education efforts of Black physicians are, they simply aren’t enough during this pandemic. The wounds the medical industry continues to cause the Black community can’t be mended through conversation and education. The entire system needs an overhaul—not to mention more Black doctors. “Instead of talking about African American behavior, we need to talk about the health-care system,” says Washington. “We need to talk about improving that system. If we have a system that’s trustworthy, people will trust it.”
Listen to a biochemist explain how vaccines work:
Sign Up for Our Daily Newsletter
Get all the latest in wellness, trends, food, fitness, beauty, and more delivered right to your inbox.
Got it, you've been added to our email list.










